Breast cancer is the most common type of cancer in women!
Approximately 1 in 8 women to 1 in 12 will be diagnosed with breast cancer during lifetime 2. 5-10% of breast cancer cases and 20% of ovarian cancer cases are hereditary3. In fact, genetic factors are incriminated for 5-15% of all cases of breast and ovarian cancer in women and for 4-40% of cases of breast cancer in men.
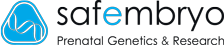
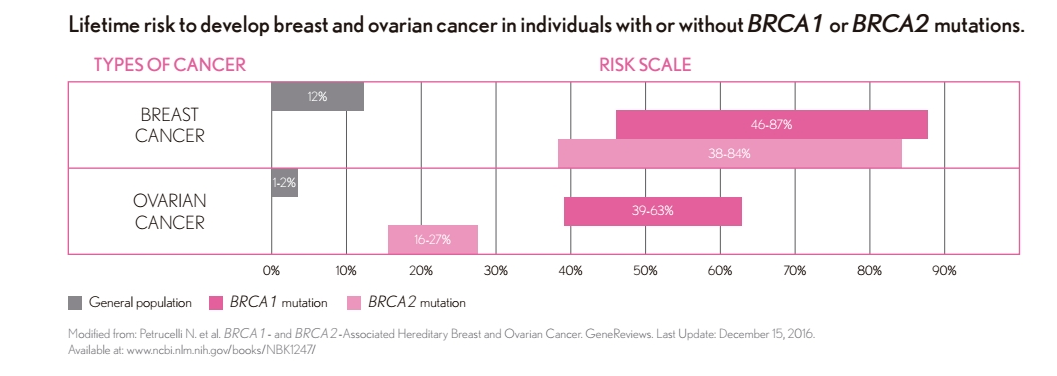
Hereditary breast and ovarian cancer is generally associated with mutations in BRCA1 and BRCA2 genes. These genes act as tumour suppressors blocking the development of cancer in normal situations. Thus, in a large proportion of the inherited forms of breast cancer, mutations occur in these two genes, whereas the carriers of these mutations are also predisposed to ovarian cancer. Approximately 50% of women with mutations in BRCA1 or BRCA2 genes do not have a family history of breast or ovarian cancer and are unaware that they are carriers of mutations that increase the risk of these types of cancer.4 Laboratory identification of inherited breast and ovarian cancer is of particular importance for the early diagnosis of the disease before the onset of symptoms, as preventive controls are intensified in these individuals, and early detection of the disease leads to increased treatment efficacy . Particularly important is the screening of BRCA1 and BRCA2 gene mutations in individuals who have already been diagnosed, as the carriers of these mutations have an increased chance of recurrence of cancer. In this way, early disease prevention, using chemoprophylaxis and / or specific surgical procedures, as well as by avoiding the exposure of a person having a family history of such cancer to hormones, e.g. administered during artificial insemination or menopause. It is equally important to avoid psychological and financial costs, as well as complications from unnecessary monitoring and / or surgical procedures, to family members who are negative for the gene mutation found in the family. Full gene screening of BRCA1 and BRCA2. The methodology used is genetic analysis of the base sequence of the BRCA1 and BRCA2 genes (DNA sequencing / Ion Torrent platform) to detect mutations associated with hereditary predisposition of breast and ovarian cancer with 99% sensitivity. In addition, the MLPA method is used to identify large genetic rearrangements (deficiencies, doubling) that deactivate the BRCA1 and BRCA2 genes. Experts worldwide recommend genetic testing of the BRCA1 and BRCA2 genes in women over 30 years of age as part of their routine examinations4. Integrated gene testing for BRCA1 and BRCA2 & 16 additional genes. In addition to the BRCA1 & 2 genes, the test includes all genes that, based on strong scientific data, are associated with breast, ovarian and endometrial cancer5-22 and require special treatment according to the National Comprehensive Cancer Network (NCCN23) guidelines. RELIABLE EASY AND SIMPLE Saliva or blood sample available COMPREHENSIVE AND SIMPLE TEST REPORT Report designed to facilitate the result interpretation. DATABASES Classification and study of variants with the most complete databases. FAST AND AFFORDABLE The high degree of automation allows to obtain results in 20 working days.
SYNLAB QUALITY AND EXPERTISE This test is performed entirely at SYNLAB’S laboratories. Developed by the genetic experts of SYNLAB group, Europe’s number one medical diagnostics provider. GENETIC COUNSELLING Safembryo offers genetic counselling before and after the results of the test. Complete screening of BRCA1 and BRCA2 & 50 more genes. In case no mutations are detected in the BRCA1 and BRCA2 genes, then you can go further and analyse another 50 genes, mutations of which are associated with increased susceptibility to breast cancer (6 genes: PTEN, CDH1, ATM, TP53, STK11, PALB2, CHEK2) or for cancer in general. The 50 genes are: ABL1 EGFR GNAS PTPN11 AKT1 ERBB2 GNAQ MET RB1 ALK PTEN HNF1A MLH1 RETAPC EZH2 HRAS MPL SMAD4 ATM IDH1 NPM1 FGFR1 JAK2 NOTCH1 BRAF FGFR2 CDKN2A FBXW7 NRAS SRC SMO FLT3 CDH1 SMARCB1 JAK3 FGFR3 VHL ERBB4 TP53 KDR STK11 CSF1R IDH2 PDGFRA CTN NB1 PIK3CA GNA11 KIT PTEN *This test is recommended as an additional screening test to BRCA1 & BRCA2 basic test Mutations have been classified and interpreted according to the guidelines of the American College of Medical Genetics and Genomics (ACMG)24. Probably pathogenic mutations: Variants probably linked to disease. Variants of uncertain significance: Variants suspected of pathogenicity without decisive evidence. No mutations detected: Mutations have not been identified. Important considerations: The presence of mutations in the genes of the panel related to breast, ovarian and endometrial cancer may also imply a higher risk for other cancer types
However, when these genes have certain mutations, they lose their functionality and cannot block or impede tumour development.
In addition to the BRCA1 and BRCA2 genes, there are other genes related to these cancer types that must be studied in order to provide a more comprehensive information than only analysing BRCA1 and BRCA2 genes, which gives the test a high reliability.Only around 25% of hereditary breast and ovarian cancer cases are due to mutations in BRCA1 and BRCA2 genes.3
Read the detailed brochure here.
or hereditary cancer syndromes (e. g. Lynch, Cowden and Li-Fraumeni syndromes). This information, if applicable, will be included on the report.